Nurse Notes
3-5-2020
Novel Coronavirus: Is a virus strain that is spread by:
By Air-coughing and sneezing close personal contact- touching or shaking hands touching an object or wet surface with the virus on it, then touching your mouth, nose or eyes in rare cases-contact with feces Good Hand washing is one of the steps to help the spreading of this virus and any illness.
2-5-2020
Secondhand Smoke
Smoking harms both you and the ones you love. Quitting smoking will benefit you plus help you protect the people in your life.

Quitting will make the people you care about happier and healthier. This may be one of your reasons for quitting.
Dangers of Secondhand Smoke
The main way smoking hurts non-smokers is through secondhand smoke. Secondhand smoke is the combination of smoke that comes from a cigarette and smoke breathed out by a smoker. When a non-smoker is around someone smoking, they breathe in secondhand smoke.
Secondhand smoke is dangerous to anyone who breathes it in. It can stay in the air for several hours after somebody smokes. Breathing secondhand smoke for even a short time can hurt your body.
Take this quiz to see how much you know about the dangers of secondhand smoke.
Health Effects of Secondhand Smoke
Over time, secondhand smoke has been associated with serious health problems in non-smokers:
Lung cancer in people who have never smoked.
More likely that someone will get heart disease‚ have a heart attack‚ and die early.
Breathing problems like coughing‚ extra phlegm‚ wheezing‚ and shortness of breath.
Secondhand smoke is especially dangerous for children, babies, and women who are pregnant:
Mothers who breathe secondhand smoke while pregnant are more likely to have babies with low birth weight.
Babies who breathe secondhand smoke after birth have more lung infections than other babies.
Secondhand smoke causes kids who already have asthma to have more frequent and severe attacks.
Children exposed to secondhand smoke are more likely to develop bronchitis, pneumonia, and ear infections and are at increased risk for sudden infant death syndrome (SIDS).
The only way to fully protect non-smokers from the dangers of secondhand smoke is to not allow smoking indoors. Separating smokers from non-smokers (like “no smoking” sections in restaurants)‚ cleaning the air‚ and airing out buildings does not get rid of secondhand smoke.
Other Ways Smoking Affects Others
Smoking affects the people in your life in other ways, beyond their health. When you smoke, you may miss out on:
Spending time with family and friends.
Having more money to spend on the people you love.
Setting a good example for your children. Children who are raised by smokers are more likely to become smokers themselves.
Steps You Can Take to Protect Your Loved Ones
The best thing you can do to protect your family from secondhand smoke is to quit smoking. Right away, you get rid of their exposure to secondhand smoke in your home and car, and reduce it anywhere else you go together.
Make sure your house and car remain smokefree. Kids breathe in secondhand smoke at home more than any other place. The same goes for many adults. Don’t allow anyone to smoke in your home or car. Setting this rule will:
Reduce the amount of secondhand smoke your family breathes in.
Help you quit smoking and stay smokefree.
Lower the chance of your child becoming a smoker.
When you’re on the go, you can still protect your family from secondhand smoke:
Make sure caretakers like nannies, babysitters, and day care staff do not smoke.
Eat at smokefree restaurants.
Avoid indoor public places that allow smoking.
Teach your children to stay away from secondhand smoke.
Find out more about secondhand smoke:
From the National Cancer Institute, Secondhand Smoke: Questions and Answers
From the Centers for Disease Control and Prevention‚ Secondhand Smoke (SHS) Facts
1-31-2020
Saturated Fat

Eating foods that contain saturated fats raises the level of cholesterol in your blood. High levels of LDL cholesterol in your blood increase your risk of heart disease and stroke.
AHA Recommendation
The American Heart Association recommends aiming for a dietary pattern that achieves 5% to 6% of calories from saturated fat.
For example, if you need about 2,000 calories a day, no more than 120 of them should come from saturated fat.
That’s about 13 grams of saturated fat per day.
What are saturated fats?
From a chemical standpoint, saturated fats are simply fat molecules that have no double bonds between carbon molecules because they are saturated with hydrogen molecules. Saturated fats are typically solid at room temperature.
How do saturated fats affect my health?
Replacing foods that are high in saturated fat with healthier options can lower blood cholesterol levels and improve lipid profiles
What foods contain saturated fat?
Saturated fats occur naturally in many foods. The majority come mainly from animal sources, including meat and dairy products.
Examples of foods with saturated fat are:
fatty beef,
lamb,
pork,
poultry with skin,
beef fat (tallow),
lard and cream,
butter,
cheese and
other dairy products made from whole or reduced-fat (2 percent) milk.
In addition, many baked goods and fried foods can contain high levels of saturated fats. Some plant-based oils, such as palm oil, palm kernel oil and coconut oil, also contain primarily saturated fats, but do not contain cholesterol.
What are alternatives to replace saturated fats in the foods I eat?
To get the nutrients you need, eat a dietary pattern that emphasizes:
low-fat dairy products,
while limiting red meat and sugary foods and beverages.
Choose lean meats and poultry without skin and prepare them without added saturated and trans fat.
You should replace foods high in saturated fats with foods high in monounsaturated and/or polyunsaturate fats. This means eating foods made with liquid vegetable oil but not tropical oils. It also means eating fish and nuts. You also might try to replace some of the meat you eat with beans or legumes.
There’s a lot of conflicting information about saturated fats. Should I eat them or not?
The American Heart Association recommends limiting saturated fats – which are found in butter, cheese, red meat and other animal-based foods. Decades of sound science has proven it can raise your “bad” cholesterol and put you at higher risk for heart disease.
The more important thing to remember is the overall dietary picture. Saturated fats are just one piece of the puzzle. In general, you can’t go wrong eating more fruits, vegetables, whole grains and fewer calories.
When you hear about the latest “diet of the day” or a new or odd-sounding theory about food, consider the source. The American Heart Association makes dietary recommendations only after carefully considering the latest scientific evidence.
11-19-19
With the winter cold and flu season imminent, you often hear advice for how to keep your family healthy. Unfortunately, even the most diligent hand-washers may become ill with cold or flu symptoms at some point, and you’ll be faced with the age-old question: when is it necessary to keep your child home from school?
CHILDREN ARE MORE LIKELY THAN ADULTS TO GET SICK AND SPREAD GERMS AND THEY EXPERIENCE LONGER RECOVERY TIMES, AND YET, PARENTS CANNOT DISCOUNT THE IMPORTANCE OF THEIR CHILD’S SCHOOL ATTENDANCE.IT IS RECOMMENDED THAT YOU KEEP YOUR CHILD HOME WHEN THEY HAVE A FEVER, VOMITING OR DIARRHEA. THESE ARE INDICATORS THAT YOUR CHILD IS CONTAGIOUS AND SHOULD MINIMIZE CONTACT WITH OTHERS. YOUR CHILD MAY RETURN TO SCHOOL AFTER THEY ARE SYMPTOM-FREE FOR A 24-HOUR PERIOD WITHOUT THE USE OF MEDICATIONS.
Masking symptoms with medications exposes others to illness and may even prolong the time your child is sick. Illnesses are generally the most contagious during the first few days. Besides the obvious indications of fever, vomiting, and diarrhea, it may be difficult to decipher your child’s symptoms to determine if they should attend school or stay home.
If your child experiences unusual tiredness with body aches, uncontrolled coughing, an unexplained rash, or a severe sore throat, they should stay home to allow for rest and a speedy recovery before they return to school.
As a caregiver to your young learner, you are the best judge of their needs. Children who are too ill to participate in learning activities in school are better assisted by taking a day or so to recoup so they may return to their classrooms healthy and ready to learn.
In the event you are having trouble deciphering your child’s illness and their ability to attend school, please call the school nurse. The nurse can be an excellent resource in determining if your child’s symptoms warrant time at home to recover. Also, when reporting your child’s absence, please detail the illness symptoms so the nurse can successfully track prevalent trends.
Help your child to recognize the symptoms of illness and set a good example by staying home and caring for yourself when you are ill. Minimizing the spread of illness protects others who may have a difficult time battling the cold or flu. Additionally, it may be helpful to plan ahead to determine how you will care for your child when they are too sick to attend school. By doing so, you will alleviate the stress of finding a caretaker at the last minute.
And remember — thorough handwashing is the most effect
10-29-19
How Parents Can Work with School Nurses to Improve Their Kid’s Health

Share on Pinterest
To help your kids through the school year, you should reach out to the school nurse before your child becomes ill.
School nurses also advise turning in key paperwork so that they are allowed to administer OTC medication in case your child becomes ill at school.
Additionally, parents of children with chronic illnesses should make a point every year of visiting to make sure everyone knows what issues the child faces.
With the cold and flu season in full swing, your child may be visiting the school nurse with symptoms.
However, in addition to managing students’ illnesses, the nurse is doing a lot more.
“We are responsible for everyone in the building — students, staff, and visitors. We’re on high alert a lot,” Robin Cogan, RN, school nurse in New Jersey and faculty member at Rutgers School of Nursing-Camden, told Healthline. “I like to call us the Chief Wellness Officer, even though we don’t officially have that title.”
From assessing illnesses and injuries to helping care for children with chronic conditions like diabetes, the nurse’s day is packed.
If you’re worried your child could be overlooked, here’s how you can work with your school nurse to ensure your child gets the support they need.
1. Build rapport
Linda Mendonca, RN, president-elect of the National Association of School Nurses, says get to know your school nurse’s name, whether your child has a chronic condition or not.
“Just because your child doesn’t plan to see the nurse regularly for a condition doesn’t mean you shouldn’t know the school nurse because there may be a time when your child doesn’t feel well,” Mendonca told Healthline.
Cogan agrees, noting that the school nurse is the key person between home and school, home and the physician’s office, and the classroom and nurse’s office.
“We are that soft place to land in the school. We don’t give grades, and the kids know there is a caring person there who can help them. Anything that a parent can share with a school nurse that will add to the success of the student is [helpful],” said Cogan.
By building a rapport, Cogan said the parent can learn what the nurse does and when and why the nurse may send a student home.
“Our goal is to keep our students safe, healthy, and ready to learn. Part of that is keeping them in their seats in the classroom,” she said.
However, when a child is injured or showing signs of illness, such as vomiting, diarrhea, or fever, they may be sent home, depending on the school’s policies.
“Some of these stomach bugs or something like strep or pink eye can run rampant through school, so part of our job is surveillance, and we have to make sure the kids in school are healthy and not contagious,” said Cogan.
2. Communicate openly
Mendonca says at the beginning of the school year, inform the nurse of anything that has happened over the summer that may impact your child, and continue to do so throughout the school year.
“Things will happen with a child over the weekend or overnight, and if it’s something the school nurse should be aware of that could possibly impact their child’s school day, it’s helpful for the nurse to know,” she said.
Because policies that determine which forms of communication (phone, text, or email) are allowed vary from school to school, Mendonca says ask your nurse which form of communication you should use.
And in addition to medical information, be sure to share experiences that may affect a child’s emotional and mental well-being.
“There was a study done that found [school nurses] spend more than 35 percent of our time on mental health issues. We find that kids will come [to us] with somatic complaints like body ache, headache, stomachache, but if you dig deeper, there may be an underlying issue like anxiety or depression, so we have to spend the time trying to understand the child through a trauma responsive lens,” said Cogan.
This may involve determining if the child is going through an experience like being bullied or dealing with family trauma, such as loss of a loved one, a parent losing a job, or parents going through a divorce.
In some instances, depending on staffing in the school, the child may be referred to a mental health professional.
“Some schools have social workers or school psychologists, and in the upper secondary schools, guidance counselors. Sometimes social workers have two schools and may not be in the school every day, but can be called for a crisis. School nurses deal with a lot of mental health issues and can counsel, but for the most part will reach out to the school psychologist or social worker who is available to help,” said Mendonca.
3. Turn in paperwork
Mendonca says sending in up-to-date paper work is essential.
“Most schools send home a health update form. Again, this varies but some schools will give [children] an over-the-counter medication like ibuprofen or antacid … but they do need a [standing doctor’s order and] parent’s permission to do that. … It’s very important that parents return [signed forms] to the school nurse so they have what they need to take care of your child,” she said.
If your child has a chronic condition, sending necessary supplies to schools should be priority. For instance, insulin or blood monitoring devices for children with diabetes, antihistamines and epinephrine for kids with allergies, and inhalers for those with asthma.
Ensuring your child is current with physicals and immunizations is also crucial, says Cogan.
“Students need proper documentation to take medication at school and on trips. Proper documentation for medication has to be signed by the doctors and parents,” Cogan said. “We don’t want to have to exclude kids [from school or attending field trips], but sometimes that exclusion date finally gets parents into action because parents have a lot going on and unless there is an impeding deadline, it can fall off their radar quickly.”
4. Advocate for our child
Because children spend much of their waking hours at school, Cogan says parents of children with chronic conditions or special needs should advocate for their safety at school.
“Have face-to-face meetings with the school nurse and teacher so we are on the same page for your child,” she said.
Each time your child switches to a new classroom, Cogan says ask for another meeting.
“Every single person who [comes in contact with] your child needs to know if they have a chronic health condition or certain medical needs. Nurses keep medical information confidential. We can only tell the staff so much because it’s private, but a parent can share as much as they want to with staff and if it comes from the parent, it’s so much more impactful,” said Cogan.
This goes for any social or emotional concerns, too. For instance, Cogan says she has had students come to her to talk about homelessness, food insecurity, gender and sexuality issues, as well as pregnancy.
“These are real life issues that come to school,” said Cogan. “Our role is all about health and safety, and the more information that we have from the expert, who is the parent, the better we can serve your child.”
10-15-19
Healthier Halloween Treats:
Cheese and cracker packages
Sugar-free gum
Small bags of pretzels or popcorn
Small packages of nuts
Peanuts in the shell
Fruit-Roll Ups
Fortune cookies
Granola bars
Go Natural: If you are not opposed to sugar, but would prefer your treats to be natural or vegan, we suggest you visit your local natural food store or go online to shop. There are a variety of natural candy companies and many of them have developed Halloween Packaging. The one drawback to natural candies is that you can expect to pay more for these items.
Tooth Fairy-Friendly: One product gaining popularity is xylitol products. Xylitol is a natural sweetener that can help reduce tooth decay. Dr. John’s Candies (http://www.drjohns.com) is one source for Xylitol candy and with a Google search, you can find others.
Homemade Treats: You could make homemade treats. Unless you are in a neighborhood with close friends, we don’t suggest this approach. Most parents go through Halloween candy and throw out unopened, unwrapped or homemade treats. If you decide to make your treats, wrap your homemade item up well, and add your name and phone number to the bag with the treat. If the parent recognizes your name, it will make them feel the treat is safe.
Alternates to Food Treats: No one said Halloween treats have to be edible. An alternative to the junk food challenge is to offer a non-food treat. Today, many families are opting for this choice. With a little bit of thought and some clever shopping, you can find some great items for a few cents per item. Here are few ideas:
Glow stick jewelry
Fortune telling Fish
Cool temporary tattoos
Scary stickers
Bouncy balls
Crayons, pencils, colored chalk
Fun erasers
Mini containers of Play-Doh
Rubber spiders, worms, or other creepy figures
Spider, skull, or pumpkin plastic rings
Check your local dollar or craft stores for fun items or shop online to have items shipped directly to you. A quick search on Google will give you plenty of online shopping choices.
08-22-19
Back to School
How can parents best work with their school nurses? We asked some nurses at last year’s training what information they’d like parents to give them and how parents can be better partners in their child’s care.
Make sure your contact information is updated online (if your district has an online emergency contact form) and also on paper (if they don’t have the online form or the power goes out).
Make sure your child knows your phone number and the phone number of a few more people to call in an emergency. It’s not enough to have it in their phone. Their phone might not be charged at that moment.
Answer the phone when the nurse calls you, and have a plan for what to do if your child needs to go home. Have a backup person who can pick up your child if you’re not available, and make sure that your backup person is on the emergency contact form.
Know that a school nurse cannot diagnose. They can make a suggestion of what they think might be going on, but you have to take your child to a doctor to receive a diagnosis and treatment. The school nurse also is not your primary care clinic. However, sometimes school nurses might notice things that a teacher or parent has not, and often, they know what ick is going around.
Follow the 24-hour fever-free rule to return to school. Our nurses understand that parents have to work, but giving a kid Tylenol or Advil to get the fever down doesn’t qualify as being 24-hours fever-free. It has to be 24 hours fever-free with no assistance. This is for your child’s safety as well as other children’s, to stop the spread of disease. Remember last year’s flu season, when some districts had classrooms with very few kids in them? Let’s try to avoid that this year.
For very young kids, put a clean pair of pants and underwear in their backpack and keep them there all year. Make sure your child and your child’s teacher know where those clothes are. Nurses often have to send kids home or find clothes in the lost-and-found or try to clean up kids after an accident.
Share medical information with the nurse. They want to know if your child has a chronic illness, what medication your child is on and how much, what food or other allergies your child has and what to do if she has an attack, and what mental health diagnoses your child might have. If you think the teacher or the counselor has this information, don’t assume it’s filtering down to the nurse. It can be beneficial to sign a record-sharing request for your child’s doctor’s office to send over medical information.
Let the nurse know if there has been flu, strep or another communicable disease. The school districts’ health departments are required to share numbers with the state and even the Centers for Disease Control and Prevention. Those numbers start with the school nurse and can help establish a pattern of where and how quickly a virus is moving.
Share the 504 plan or individualized education plan with the nurse. The teachers, counselors and administration might know it, but the nurse also should be informed, especially if it’s for behavior, physical health or mental health. They want to know what works with your child. They also want to know if the behavior that has caused your child to go to the nurse is normal for them. If your child regularly has panic attacks, that’s helpful for the nurse to know if your child comes in with shortness of breath.
Let the nurse know about a long-term medical condition that might mean homebound services will be needed. Sometimes the school nurse gets tasked in getting assignments for kids who can’t attend school.
Have the right paperwork for giving a child medication. If your child needs to take medicine while at school, most districts won’t let you just give the kid the pill bottle. There will be paperwork involved that comes from your doctor if it’s prescribed or from you if it’s over the counter. Each district has its own set of guidelines. Ask your nurse what you need to provide, and know that she can’t give your child anything if the paperwork is not filled out properly.
Realize that kids are different at school than at home. Sometimes kids will have stomachaches and headaches at school and be fine at home, or the opposite can be true. It depends on how your child is wired. Recognize that the symptoms the nurse sees might not be the same symptoms you see regularly.
Understand that the nurse might not need to call you. Most districts have protocols for calling parents if there is a fever or head injury. If there’s an injury that seems to be fixed with a bandage or if the kid just needs a break, the nurse might not call you. Sometimes nurses who know families well have more information about whether you’re the kind of parent who wants a call at every visit to the nurse’s office. If you are that parent, let the nurse know you’d like a call. Realize that the nurse’s time is valuable (usually there’s only one of her for hundreds or even thousands of children). She might not be able to call you that moment. A good reason you might want a call is if you’re trying to establish a pattern to your child’s symptoms or if you’re trying out a new medication and need to know if it’s working.
When in doubt, overshare information. Often the school nurse is the last to know but the first to see your child in an emergency.
03-07-19
Beyond Chicken Nuggets: Protein-Rich Alternatives for Picky Eaters

By: Claire McCarthy, MD, FAAP
All parents want their children to have healthy diets—and part of that is getting enough protein. With picky eaters, that can feel hard. But it doesn’t have to be hard.
Here are some things about protein that you may not know—and some ideas to make mealtimes easier.
When all your child will eat is chicken nuggets:
As a pediatrician, I talk with parents all the time about what their children eat. And very often I find that when it comes to giving their children protein, families feel frustrated—and worried. “All he will eat is chicken nuggets” is something I commonly hear.
When babies are small it’s not really an issue, because they are on breast milk orformula. But as they grow into toddlers and preschoolers and we expand their diets, that’s where the worry sets in—because the age when they are expanding their diets is also the same age when they become more independent and willful. It’s a power struggle that often plays out as picky eating.
Enter the chicken nugget. I’m not sure what it is about them that makes kids almost universally like them; perhaps it’s the same thing that makes French fries universally appealing. Some even look like French fries. And for many families it can seem like once you’ve started the “nugget habit,” there’s no turning back. But here’s the thing: you don’t need to start that habit. And for those of you already in the habit, there is hope.
Why protein is an important part of your child’s diet:
When we think of protein we think of muscles, but protein is a building block for many other parts of the body, such as hair, bones, enzymes, skin and blood. Our bodies are very good at recycling and reusing proteins as they break down, but we do need to get some from our diet.
Here are three things about protein that many parents don’t know:
1. Children don’t need as much protein as you might think. The body is remarkably good at recycling.
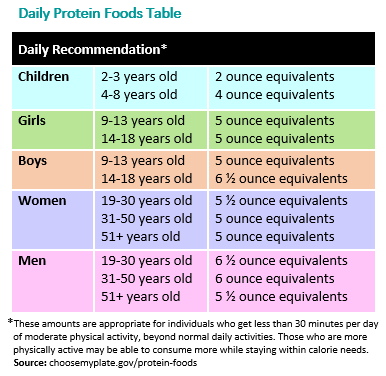
2. If children are drinking the recommended amount of cow’s milk, they are likely getting all or most of the protein they need. Every ounce of cow’s milk has 1g of protein; soy and plant-based milks do not.
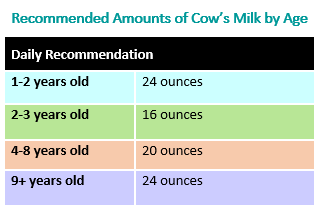
If you compare this to the recommended amounts of protein above, you’ll see that milk alone could take care of all a child’s protein needs until age 9! Hopefully, that eases some parents’ worries. After age 9, your child is hopefully old enough to negotiate about healthy food choices.
It’s certainly true that some children don’t like milk, and that drinking more than the recommended amount can lead toconstipation or anemia (and sometimes poor eating habits when children want milk instead of food). Which leads to the third point…
3. There are lots of ways besides meat or cow’s milk to get protein and mix it up at mealtime. Here are some other protein-rich ideas.
Other animal products. Salmon, fish sticks, eggs, turkey lunch meat, yogurt, or mozzarella string cheese.
Beans and grains. Soy products like soy milk or tofu. (You can even try soy “chicken” nuggets). Lentils, nut butter, hummus, oatmeal, or whole wheat pasta are more options.
Vegetables. Yet another reason to get kids to eat their veggies! Peas, broccoli, and even potatoes have protein. (Not that potatoes are the best vegetable, but it’s good to know they have some protein).
The bottom line:
When it comes to getting protein into your child’s diet, you don’t have to get into battles—or give in to the daily chicken nugget diet. There are lots of ways to do it, and with a bit of creativity and persistence, your child can get what he or she needs.
No clean-plate club. Don’t force your kids to eat something or finish everything, because that doesn’t work well (and makes everyone miserable). Kids don’t need a balanced meal at every meal of the day―what’s important is achieving balance over a day or two.
Keep it on the plate; have a “one bite” rule. It can take lots of tries before a child realizes that something tastes good. It also helps when others set an example, so eat meals together whenever you can!
Cook more meals at home. A homemade breaded chicken breast, for example, is healthier than takeout nuggets. Kids learn a lot about different foods and how to read food labels when they are involved in shopping for groceries and preparing meals―making them into healthier adults. Here are five more great reasons to cook with your kids.
If nothing is working, or you are worried about your child’s diet, call your doctor.
Yes, picky eating can just be a phase. But it’s important to bring up any concerns with your pediatrician, so you can brainstorm possible solutions together.
01-31-19
Surviving the Stomach Bug: Truths & Tips for Parents

Stomach bugs tend to be the nastiest illnesses our children bring home from school.
7 Truths & Tips for Survival of Stomach Bugs When They Hit Your Home
Hand washing and keeping things clean are your best defenses from getting ill with a stomach bug. Not surprisingly, this is particularly true after touching or supporting your child and when preparing food and eating. Some viruses will survive on surfaces for days. And some viruses like Norovirus can even survive hand sanitizer. You have to use soap and water to kill it. But even with ridiculous, meticulous attention to hygiene, every parent knows that when the vomit is flying, it’s hard to lasso every single errant particle. So simply commit to do your best. Change the sheets and clean up areas of vomit immediately after supporting your child. Soapy warm water is your friend. Wash surfaces immediately, use hot water for the wash, and use high heat in the dryer.
24 hours (or so): In general, most pediatricians will tell you that vomiting doesn’t exceed 24 hours with typical gastroenteritis. Occasionally it can. Many kids don’t follow the rules. Once a virus that causes gastroenteritis takes hold of a child, vomiting starts. Children tend to vomit more than adults. Part may be an easy gag reflex. With most viruses that cause the “stomach flu,” as the infection moves through the stomach and intestines, vomiting stops after about 24 hours. But not always. If you advance liquids too quickly or children eat more solids than they are ready for, even after the first meal 1 to 2 days into eating again, they may have a vomit encore. If you have one of those, start back where you started (sips of clear liquids) and go very slow advancing their diet. If vomiting is accelerating at 24 hours, it is time to check in with your child’s doctor.
Disgusting and terrifying: It’s creepy-eepy to take care of a child with vomiting. Not only is it entirely gnarly and disgusting to remove and clean chunks from vomit-laden carpet, sheets, and clothing, it’s also terrifying to provide support to a vomiting child because you can get equally uneasy about catching the virus. You’re not alone in this. It’s absolutely nauseating to see your own child ill, unwell, and retching. And it’s awful to imagine having to provide care while getting miserably sick. Do your best to keep your hands washed and keep the love going. As all of us know, when you find yourself picking out vomit bits from the carpet at 3:00 am, it really can only get better from there.
Medication: Children rarely need medication when recovering from gastroenteritis. Although some antinausea drugs are available for use in children, most children don’t need prescription medications. Talk with your child’s pediatrician if you feel you child is vomiting longer than 24 hours or becoming dehydrated. Remember that vomiting is a protection reaction of your child’s body to clear infection.
Soap, water, and bleach: William Osler said, “Soap and water and common sense are the best disinfectants.” Cleaning your home to avoid spreading infection is a must. You don’t need expensive products, just vigilance. With some highly infectious viruses that cause vomiting, even 10 viral particles can cause illness. So in addition to soap and water, consider using a dilute bleach solution to clean hard surfaces.
Detective work: Sometimes you’ll simply never know where it all came from. But it won’t stop you from playing the role of infectious detective. The only issue: this is simply wasted time.
Yummy, clingy love: There is an occasional perk to a terrible stomach bug. And we have to find one to maintain a sense of optimism. When our children are ill, they really turn over and show us they want us over anything else on earth.
Then there is resilience. Children do very well recovering from typical viral gastroenteritis, although diarrhea can last for days. Even so, our children’s resilience will long astonish us.
01-09-19
Is Your Child Getting Enough Sleep to Perform at His or Her Best? How Kids Can Sleep Smarter and Perform Better
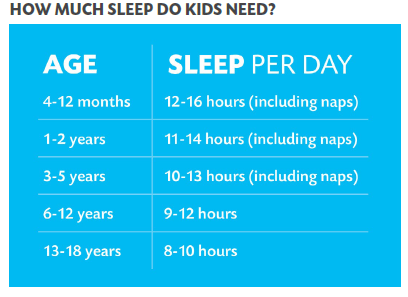
Kids know they should eat well and be physically active, but they don’t always understand that healthy sleep is also an important part of a healthy lifestyle. And while they often wish they were getting more sleep, they report sleep as the lowest scoring health item for things that are important for their well-being. In fact, did you know that 71 percent of students are sleep deprived by an average of 1.7 hours a night1?
Let’s do the Math: How Sleep Affects Academic Performance and Achievement
Research shows that students need at least 8 hours of shuteye each night2 . But if they are not hitting the hay before 10:30 p.m. on school nights – and they have to be out the door by 7:15 a.m. (or earlier) to get to school – that’s less than the minimum hours needed for winding down, getting to sleep, and then getting ready for school in the morning.
Chronic sleep deprivation is a real problem. It’s not simply too much screen time or social media that’s to blame. Kids are staying up later and getting up earlier because school days are longer and they have more work to manage in a shorter amount of time outside the school bells. This cycle is stressful for students.
What Do Our Kids Think Could Help?
A 2018 survey, conducted by GENYOUth in partnership with Sleep Number, found that 42 percent of students say they don’t get enough sleep because of things they have to do, like homework, compared to 22 percent who report that it’s due to things they choose to do. We might think that students believe that less time on social media would result in more sleep. The reality? Kids believe help managing their time is the answer.
More than half sleep-deprived students believe they would handle stress better and do better in school if they got more vitamin ZZZ. Furthermore, students with higher grades are getting more sleep each night than those with lower grades.
Adults can help their kids be less busy and teach and support good sleep habits, such as bedtime routine.
Bed Times Matter!
According to the GENYOUth survey, 60 percent of students who get eight or more hours of sleep go to bed around the same time each night. Students who do not have a regular bedtime, about one-third of the survey respondents, get six or less hours of snooze time. Students with a set bedtime usually go to sleep around 10:00 p.m. Those without, on average, go to bed around 11:00 p.m. and are more likely to stay up past midnight.
So how much is enough? Is your child getting the adequate amount of quality sleep? Check out the American Academy of Sleep Medicine’s recommendations3.
Tips for Taming Your Child’s Sweet Tooth in a World of Sugary Treats:
Take stock of sugar. In order to know how much added sugar is in food, it’s important to be able to spot it on a label. Current food labels display total sugar—which includes natural sugars like those found in an apple—and may or may not include any added sugars used to enhance flavor. On average, Americans get about 13% of their total calories from added sugars, with the major sources being sugar-sweetened beverages and snacks and sweets. By July 2018, however, food labels must display “Includes X g Added Sugars” under “Total Sugars.” This change makes it easier for parents to understand how much sugar has been added to a product. See Changes to the Nutrition Facts Label: What Parents Need to Know for more information and a side-by-side comparison of the original and new labels. It also helps to know the conversion of sugar from grams to teaspoons (i.e., 4 grams = 1 teaspoon). In a 2,000-calorie-a-day diet, for example, 10% would be equal to about 50 grams of sugar (or 10 teaspoons).
Spot “sneaky” sugar. Many foods that are marketed as “health foods” can actually have a lot of added sugar. Always check the labels on sports drinks, smoothies, protein and granola bars, and yogurt; some can have as much as 4 to 5 teaspoons of added sugar per serving. Whole fruit makes a great substitute for these items and counts as dessert, too. If your kids balk at first (and they will), melt some dark chocolate and let your kids dip—and what kid doesn’t love to dip! Dark chocolate actually contains 70% cocoa and has less than half the sugar of milk chocolate.
Keep beverages simple. Stick with milk (including non-dairy milk) and water as your child’s main beverages. While the American Academy of Pediatrics (AAP) does suggest 100% fruit juice can be an acceptable part of a healthy diet, be aware that it’s wise to offer it in age-appropriate moderation (none routinely under 12 months of age and no more than 4 oz. per day for 1 to 3 year old children or 4 to 6 oz. for 4 to 6 year old children). In reality, it can be challenging to limit once kids get used to the sweetness. An alternative to juice would be to place sliced fruit into water to give it some flavor without the excess sugar. Also avoid letting your child sip on juice (or any other sugar-containing liquid, for that matter) for long periods. Whether by bottle, sippy cup, box, or cup, bathing one’s teeth in sugary liquids can cause serious tooth decay.
Avoid rewards with sugar. Whether it’s at home, in the classroom, or on the sports field, far too often kids are rewarded for good behavior with sugary treats. In the quest to coax kids to eat better, parents may reward “one more bite of peas” with a sweet treat. While these kind of rewards may work in the short term, it becomes a problem when children learn to expect a reward for appropriate behavior. A few sweets may turn into expectations for larger rewards like cell phones and designer clothes as children turn into teens. Consider yourself warned!
Change the culture. Far too often we celebrate holidays, birthdays, and other special occasions with sweets—making it challenging to curtail our kids’ (and our own) cravings. However, kids value other “treats” just as much as sugary ones. With some creativity many of the sugary celebrations can be reinvented with new, healthier traditions. Talk to the teachers at your child’s school, their coaches, scoutmasters, and other parents to come up with ways to celebrate with more fun and less sugar. If your child’s sports team provides sweet treats after games, for example, suggest to the coaches that whole fruit may be a healthier alternative. In addition, plain water is the best drink for most children engaging in routine physical activity; the AAP clinical report on the subject says kids should not consume energy drinks and rarely need sports drinks.
Find balance. Although we would like our kids to stay away from sugary treats as much as possible, we also want them to learn how to balance all the available choices when they are able to make food decisions for themselves. Keeping sugary treats under lock and key—or banning them all together—may also fuel an unhealthy craving for sugar. Show your children that an occasional dessert or sweet treat can be part of a balanced diet; model that behavior yourself! Sweets and snacks in appropriate portions are OK in moderation.
By being educated about sugar intake and making the occasional sugary treat a part of your family’s culture, you may find your children craving sugary treats and snacks less and enjoying them in a more mindful and balanced way for life.
10-02-18
Preventing the Flu: Resources for Parents & Child Care Providers

Parents and child care providers can help prevent and slow the spread of the flu. The flu (influenza) is a respiratory illness caused by a virus. Flu infections are highly contagious. They spread easily when children are in a group with other children such as in a child care center or family child care home.
Flu is more dangerous than the common cold for children and can lead to serious health conditions like pneumonia or bacterial infections. Each year many children are hospitalized and some die from the flu.
The following resources provide information on preventing the flu. Materials and tools for child care facilities are also included.
Protecting Children with Chronic Health Conditions
Children and adolescents with a chronic health condition, such asthma, heart disease, diabetes and disorders of the brain or nervous system are at high risk for flu complications.
Flu Vaccine Information
The flu vaccine is the best way to protect against getting the flu. All people 6 months and older need a flu vaccine each year. Babies cannot get vaccinated until they are 6 months old. It is critical that people who live with or care for children, especially newborns and infants younger than 6 months, get vaccinated. Vaccinating adults who are around an infant to prevent illnesses is often referred to as “cocooning.”
Fighting Germs
A few minutes killing germs can go a long way toward keeping you and those around you healthy. As adults, we know to wash our hands often with soap and water, especially after coughing, sneezing, or wiping noses. When you cough or sneeze, cough into your sleeve or arm or into a tissue. Be sure to dispose of the tissue and wash your hands. Parents and child care providers can do their part to kill germs and also teach young children how and when to wash their hands.
Preventing the Spread of Illness in Child Care
Young children who have just entered child care are more vulnerable to infectious diseases. This is because it may be the first time they have been exposed to certain germs. In addition, they may be too young to have received enough doses of recommended vaccines to have developed immunity.
There are steps that caregivers and teachers can take to prevent the spread of infection in child care.
How Sick is Too Sick?
When children are healthy, they can go to child care or school, and parents can go to work. Getting the flu vaccine is the best way to make sure everyone can continue to participate in these important activities. However, when a child feels too sick to participate in activities, or requires care beyond what the caregivers can provide without compromising their ability to care for other children, that child will need to stay home.
09-04-18

Four Hidden Signs of Vision Problems in Ki
Written By: Kierstan Boyd
As summer winds down, families of school-aged children scramble to get backpacks, clothes and other supplies ready for the new school year. But one of the most important yet often overlooked necessities is healthy vision.
As children grow and change from year to year, so do their eyes and vision. School demands intense visual involvement, including reading, writing, computer and chalkboard/smartboard work. Even physical education and sports require strong vision. If their eyes aren’t up to the task, a child may feel tired, have trouble concentrating, and have problems in school.
Sometimes parents can tell if their child has a vision problem. For instance, their child may squint, hold reading material very close to their face, or complain about things appearing blurry. However, there are some less obvious signs of vision problems.
Here are four signs that could point to possible vision problems in kids.

Having a short attention span.
Your child might seem to quickly lose interest in games, projects or activities that require using their eyes for an extended period of time.
Losing their place when reading.
As your child reads (aloud or silently), they may have difficulty seeing to keep track of where they are on the page.

Avoiding reading and other close activities.
Whether they are subtle or obvious about it, your child may choose to avoid reading, drawing, playing games or doing other projects that require focusing up close.

Turning their head to the side.
A child may turn their head to the side when looking at something in front of them. This may be a sign of a refractive error, including astigmatism. Turning their head helps the child see better.
Success in school is closely tied to eye health. That’s why it is so important for kids to have regular eye screenings with an ophthalmologist or another professional who is properly trained to assess vision in school-aged children. The earlier a vision problem is found and treated, the better off your child will be—in and out of school.

If you have any questions or concerns about your child’s vision, be sure to ask your child’s doctor.
We will be testing vision and hearing on September 11,2018. The above is an article I thought as a parent you may find interesting.
Thanks !
Nurse Melanie
05-01-18
From the National Council of Skin Cancer Prevention:
www.skincancerprevention.org
Don’t Fry Day
Main Message: The Friday before Memorial Day is Don’t Fry Day: Protect your skin today and every
day. Millions of Americans will enjoy the great outdoors this weekend. Skin cancer, caused by too much sun,
is the most common of all cancers in the United States. More people will be diagnosed with skin cancer
this year than breast, prostate, lung, and colon cancer combined. The National Council on Skin Cancer Prevention reminds you to enjoy the outdoors safely. We have
named the Friday before Memorial Day Don’t Fry Day. In the same way we teach kids to wear bike
helmets, we can also teach them to wear wide-brimmed hats. What You Can Do to Be Safe in the Sun:
1. Do Not Burn
Overexposure to the sun is the most preventable risk factor for skin cancer.
2. Avoid Sun Tanning and Tanning Beds
Ultraviolet (UV) light from tanning beds and the sun causes skin cancer and wrinkling. If you want to
look like you’ve been in the sun, use a sunless self-tanning product instead.
3. Cover Up
Wear protective clothing, such as a long-sleeved shirt, pants, a wide-brimmed hat, and sunglasses,
where possible.
4. Seek Shade/Use Umbrellas
Seek shade when appropriate. Remember that the sun’s UV rays are strongest between 10 a.m. and
4p.m.
5. Generously Apply Sunscreen
Generously apply sunscreen to all exposed skin using a Sun Protection Factor (SPF) of at least 30 that
provides broad-spectrum protection from both UVA and UVB rays. Reapply every two hours, even
on cloudy days, and after swimming or sweating.
6. Use Extra Caution Near Water, Snow and Sand
Water, snow and sand reflect the damaging rays of the sun, which can increase your chance of
sunburn.
7. Check the UV Index
The UV Index provides important information to help you plan your outdoor activities in ways that
prevent overexposure to the sun. Developed by the National Weather Service (NWS) and EPA, you
can find the UV Index for your area online at: http://www.epa.gov/sunwise/uvindex.html.
8. Get Vitamin D Safely
Get vitamin D safely through a diet that includes vitamin supplements and foods fortified with
vitamin D. Don’t seek the sun or indoor tanning.
Email: dontfryday@skincancerprevention.org
04-24-18
Summer Safety:
Sun Protection and Heat Exhaustion
First, avoid being in the sun between 10 a.m. and 3 p.m., and stay in a shaded area as much as possible when outside. Dress baby in a hat, sunglasses, and clothing made with a tight weave. For babies 6 months and older, use sunscreen with an SPF of at least 15 (SPF 30 and higher is even better) that offers both UVA and UVB protection. For babies younger than 6 months, if adequate shade isn’t available, put sunscreen in small amounts on exposed surfaces of skin. Always apply sunscreen at least 30 minutes before going outside — even on cloudy days — and reapply it every two hours. Even waterproof sunscreen loses its effectiveness after about 80 minutes of swimming.
How to Treat: If your child does get a sunburn, the best remedies are cold compresses, over-the-counter pain relievers, and aloe preparations.
Keep Kids Cool
As temperatures rise, heat exhaustion becomes a concern. Symptoms include fatigue, extreme thirst, and muscle cramping. If a person doesn’t cool down and rehydrate herself, heat exhaustion can lead to heatstroke (signs are headaches, dizziness, nausea, vomiting, and lack of sweat), which is potentially fatal.
How to Treat: If you notice heat illnesses in kids, spray them with cold water from a bottle or hose, fan them, and get them into the shade. Ice packs to the groin and armpits can speed up the cooling process even more. If you suspect heatstroke, call 911: Infants are vulnerable to heat-related illness, so keep them in air-conditioned areas when possible. And never leave kids in unattended cars, even with the windows cracked.
Use Caution When in Water
Sadly, drowning is among the leading causes of accidental death in children. The American Academy of Pediatrics says parents should not enroll children under age 4 in formal swimming lessons that teach water survival skills. If you want them to play in water, supervise them within arm’s reach, even in shallow water.
Special Concerns: When choosing a flotation device, go for a child-size life vest. Little arms are less likely to slip out than they are with water wings. And when compared with using a swim ring, there’s less chance of tipping over. Also, take a CPR course (find your local American Red Cross chapter at redcross.org) so you’ll be prepared in case of a near-drowning incident.
Poisonous Plants
To further help you sidestep these summer spoilers, here’s information on recognizing these plants: Poison ivy grows as a vine or shrub in the grass or on trees. Poison oak grows only as a shrub, usually in the western United States. Poison sumac is a tall shrub or small tree found in wooded areas of eastern states.
The good news: the rashes (caused by oils from these plants) aren’t contagious. Once the skin has been washed and clothing is removed, the rashes can’t spread.
Poison Ivy — Look for three pointed, notched leaves per stem.
Poison Sumac — Six to 12 leaves grow in pairs with a single leaf topping stems.
Poison Oak — Looks like poison ivy, but tips of leaves are rounded.
How to Treat: If your child’s skin comes in contact with one of these plants, you have a window of about 10 minutes to wash away the rash-causing oil. If you don’t catch it in time, a rash may develop within 12 hours. Use topical hydrocortisone cream and an oral antihistamine to calm the itch.
Special Concerns: If the rash involves the eyes or if it covers a large portion of her body, contact your pediatrician. Oral steroids may be recommended for severe cases.
Beware of Bee Stings
Bees are attracted to flowers, so don’t put fragrances or floral-patterned clothing on kids. Likewise, don’t leave out open containers of food and drink, and if your kid’s clothes get stained, change them. Should a bee land on or next to your child, remain calm and gently blow it away.
How to Treat: If your child gets stung, brush the stinger away with the edge of a credit card. Next, apply a salve of one part meat tenderizer to four parts water and leave it on the area for about 30 minutes to neutralize the venom. Then apply cold compresses and topical hydrocortisone cream, and give an oral antihistamine to reduce swelling. You could also apply a paste of baking soda and water.
Special Concerns: Bee stings often look worse the next day — skin reactions are normal and may last up to a week. But some people have severe allergic reactions to bee stings that include all-over hives, difficulty breathing, dizziness or fainting, and swelling of the lips and tongue. These can be life-threatening reactions that require immediate medical help. If your child has this allergy, his doctor will prescribe an injectable form of epinephrine, a lifesaving medicine.
Bug Bites
When outside, cover children with lightweight clothing and use mosquito netting over strollers and infant seats. Ticks are also a concern, so check your child’s body for them at the end of each day spent outside.
When choosing bug repellents this summer, know that the most effective products contain DEET because it’s proven to repel both mosquitoes and ticks. Products with a DEET concentration of less than 30 percent are safe for kids, but not for babies under 2 months old. Apply the repellent once a day and don’t use combination sunscreen/bug repellent products. All-natural repellents, such as lemon eucalyptus and citronella, aren’t proven to protect against ticks, nor should they be used in children younger than 3 years. It’s safe to apply them on older kids.
How to Treat: Topical antihistamine preparations can help relieve the itch of mosquito bites. If you find a tick on your kid, use tweezers to pull it off by its head. Ticks have to be embedded in the skin for about 24 hours to transmit germs. If you suspect a tick has been on your child for this long, contact your pediatrician.
First-Aid Kit Essentials
What better time to stock a first-aid kit than at the start of the summer season, when many accidents occur. While you can’t prevent all accidents, you can be prepared. Here is a list of helpful things to include:
Band-Aids
Soap
Antibacterial gel or foam
Triple-antibiotic ointment
Hydrocortisone cream
Sterile gauze pads
Adhesive tape
Tweezers
Washcloths
Cold packs
Infant and children’s Motrin or Tylenol
Oral antihistamine
Rubbing alcohol
Digital thermometer
Copyright © 2008 Meredith Corporation. Originally published in June 2007 issue of American Baby magazine.
Remember if you need immunization before school starts, get them over the summer!
04-03-18
YMCA Camp Lakewood is having 2018 Asthma Camp. Camp Catch-Ya_Breath in Potosi, Mo. Friday June 15-17. If anyone is interested it is a free camp for children with asthma and I have the information an the applications. They can also go on line at http://shp.missouri.edu/rt/asthma.camp.php.
If you have any questions please feel free to call 573-637-2201.
03-16-18
What to do in a Poisoning Emergency

Children can get very sick if they come in contact with medicines, household products, pesticides, chemicals, or cosmetics. This can happen at any age and can cause serious reactions. However, most children who come in contact with these things are not permanently hurt if they are treated right away.
Poison Help
1-800-222-1222 is a nationwide toll-free number that directs your call to your local poison center.
Call 1-800-222-1222 if you have a poison emergency. This number will connect you right away to your nearest poison center. A poison expert in your area is available 24 hours a day, 7 days a week. Also call if you have a question about a poison or poison prevention. You can find prevention information at http://poisonhelp.hrsa.gov.
Be prepared. Post the Poison Help number by every phone in your home and program the number in your cell phone. Be sure that caregivers and babysitters know this number.
Treatment
Swallowed poison
If you find your child with an open or empty container of a dangerous nonfood item, your child may have been poisoned. Stay calm and act quickly.
First, get the item away from your child. If there is still some in your child’s mouth, make him spit it out or remove it with your fingers. Keep this material along with anything else that might help determine what your child swallowed.
Do not make your child vomit because it may cause more damage.
If your child is unconscious, not breathing, or having convulsions or seizures, call 911 or your local emergency number right away.
If your child does not have these symptoms, call the Poison Help number, 1-800-222-1222. You may be asked for the following information:
Your name and phone number
Your child’s name, age, and weight
Any medical conditions your child has
Any medicine your child is taking
The name of the item your child swallowed (Read it off the container and spell it.)
The time your child swallowed the item (or when you found your child), and the amount you think was swallowed
If the poison is very dangerous, or if your child is very young, you may be told to take him to the nearest hospital. If your child is not in danger, the Poison Help staff will tell you what to do to help your child at home.
Poison on the skin
If your child spills a dangerous chemical on her body, remove her clothes and rinse the skin with room-temperature water for at least 15 minutes, even if your child resists. Then call Poison Help at 1-800-222-1222. Do not use ointments or grease.
Poison in the eye
Flush your child’s eye by holding the eyelid open and pouring a steady stream of room-temperature water into the inner corner. It is easier if another adult holds your child while you rinse the eye. If another adult is not around, wrap your child tightly in a towel and clamp him under one arm. Then you will have one hand free to hold the eyelid open and the other to pour in the water. Continue flushing the eye for 15 minutes. Then call the Poison Help number, 1-800-222-1222. Do not use an eyecup, eyedrops, or ointment unless Poison Help staff tells you to.
Poisonous fumes
In the home, poisonous fumes can come from:
A car running in a closed garage
Leaky gas vents
Wood, coal, or kerosene stoves that are not working right
Space heaters, ovens, stoves, or water heaters that use gas
If your child is exposed to fumes or gases, have her breathe fresh air right away. If she is breathing, call the Poison Help number, 1-800-222-1222, and ask about what to do next. If she has stopped breathing, start cardiopulmonary resuscitation (CPR) and do not stop until she breathes on her own or someone else can take over. If you can, have someone call 911 right away. If you are alone, wait until your child is breathing, or after 1 minute of CPR, then call 911.
Remember
You can help make your home poison-safe by doing the following:
Keep all medicines and household products locked up and out of your child’s reach.
Use safety latches on drawers and cabinets where you keep objects that may be dangerous to your child.
Be prepared for a poisoning emergency. Post the Poison Help number by every phone in your home and program the number in your cell phone. 1-800-222-1222 will connect you right away to your nearest poison center. (Be sure that your babysitter knows this number.)
02-22-18
Why Most Sore Throats, Coughs & Runny Noses Don’t Need Antibiotics

If your child has a sore throat, cough, or runny nose, you might expect the doctor to prescribe antibiotics. But most of the time, children don’t need antibiotics to treat a respiratory illness. In fact, antibiotics can do more harm than good. Here’s why:
Antibiotics fight bacteria, not viruses.
If your child has a bacterial infection, antibiotics may help. But if your child has a virus, antibiotics will not help your child feel better or keep others from getting sick.
The common cold and flu are both viruses.
Chest colds, such as bronchitis, are also usually caused by viruses. Bronchitis is a cough with a lot of thick, sticky phlegm or mucus. Cigarette smoke and particles in the air can also cause bronchitis. But bacteria are not usually the cause.
Most sinus infections (sinusitis) are also caused by viruses. The symptoms are a lot of mucus in the nose and post-nasal drip. Mucus that is colored does not necessarily mean your child has a bacterial infection.
Antibiotics do not help treat viruses and some infections.
Some cases of the flu are both viral and bacterial. For these cases, antibiotics may be needed. Sometimes bacteria can cause sinus infections, but even then the infection usually clears up on its own in a week or so. Many common ear infections also clear up on their own without antibiotics.
Some sore throats, like strep throat, are bacterial infections. Symptoms include fever, redness, and trouble swallowing. However, most children who have these symptoms do not have strep throat. Your child should have a strep test to confirm that it’s strep, and then, if they’re needed, the doctor will prescribe antibiotics.
Antibiotics have risks.
Side effects from antibiotics are a common reason that children go to the emergency room. These medicines can cause diarrhea or vomiting, and about 5 in 100 children have allergies to them. Some allergic reactions can be serious and life threatening. The misuse and overuse of antibiotics encourages bacteria to change, so that medicines don’t work as well to get rid of them. This is called “antibiotic resistance.” When bacteria are resistant to the medicines used to treat them, it’s easier for infections to spread from person to person. Antibiotic-resistant infections are also more expensive to treat and harder to cure.
When used incorrectly, antibiotics waste money.
Most antibiotics do not cost a lot. But money spent on medicines that are not needed is money wasted. In severe cases, infections that are resistant to antibiotics can cost thousands of dollars to treat.
When does your child need antibiotics?
Your child may need antibiotics if:
A cough does not get better in 14 days.
A bacterial form of pneumonia or whooping cough (pertussis) is diagnosed.
Symptoms of a sinus infection do not get better in 10 days, or they get better and then worse again.
Your child has a yellow-green nasal discharge and a fever of at least 102° F for several days in a row.
Your child has strep throat, based on a rapid strep test or a throat culture. If strep is not diagnosed with a test, antibiotics should not be given. No test is needed if your child has a runny nose and cough as well as a sore throat. Those are symptoms of a different virus.
For infants younger than 3 months of age, call your pediatrician for any fever above 100.4° F. Very young infants can have serious infections that might need antibiotics.
11-28-17
How Do You Get Rid Of Mucus?
Snot Color #1: Clear, Runny Mucus
Morgan Swofford for LittleThings
Clear mucus is nothing to worry about. This is the run-of-the-mill mucus your body always needs you to produce, so don’t be concerned if you notice a bit of this clear goo on your tissue.
At times, your body might suddenly start producing a lot of clear mucus, and that can be an important sign.
For example, people with respiratory allergies like hay fever may discover that their noses suddenly start running like a tap, producing huge quantities of clear, liquid snot.
That’s a good indicator that you are too close to an allergen and are about to start suffering more extensive symptoms.
It may also indicate other early respiratory issues, like the start of an ordinary cold.
Snot Color #2: Thick, White Mucus
Morgan Swofford for LittleThings
If your snot is coming out white and sticky, that means that there’s less water in the mucus than there normally should be.
Having white, thick mucus can often indicate that you’re dehydrated and that you need to get more water into your system.
If you’re getting plenty of water, it could signal that something else in your body is causing dehydration, like a low-grade fever that makes you sweat.
White mucus can also mean that a cold or sinus infection is starting to develop. When white blood cells start to build up in mucus to fight an infection, they can turn the sputum milky white.
Snot Color #3: Yellow Mucus
Morgan Swofford for LittleThings
Got yellowish or creamy colored mucus? That’s a sure sign that something is brewing in your upper respiratory system.
If you have an infection, a cold, or even a really bad allergy, your body will respond by producing lots of white cells to fight off the attacker.
White blood cells have a greenish tint, and in a low concentration, they can give clear or white mucus a yellowish hue.
Snot Color #4: Green Mucus
Morgan Swofford for LittleThings
Green mucus is a great indicator that you have a bug that is settling in for the long haul.
If you start blowing out green mucus, this could signal that an intense sinus infection might be getting its hooks into you.
Finding green mucus in your tissue is a sign that you should visit the doctor.
You should also be especially careful to watch out for green mucus that comes up from the throat and lungs.
Coughing up wads of green goo can mean that you have something like bronchitis and pneumonia brewing. Both conditions are serious and require a visit to the doctor.
Snot Color #5: Red Or Pink Mucus
Morgan Swofford for LittleThings
Red or pink mucus almost always means that you have blood in your respiratory system — but don’t panic!
It’s really easy to end up with pinkish mucus or bright-red blood in your tissue, especially if you’ve been blowing your nose a lot or have been trying to clear it of goop. The membranes get irritated and dry, and small blood vessels can break and cause the alarming color.
However, be very carefully if you experience excessive bleeding.
Contact your doctor right away should you start coughing or sneezing out large amounts of blood. If the bleeding will not stop, go to the emergency room immediately.
Snot Color #6: Brown Mucus
Morgan Swofford for LittleThings
Though mucus is not a pleasant sight, it’s generally nothing to worry about.
Usually, if you find that your mucus has a brownish color, it’s because there is old, dried blood somewhere in your nose or your sinuses.
If you previously experienced a nose bleed or a similar nasal injury, it’s not uncommon to have old brownish blood surface after the fact.
Mucus that has been backed up for a long time, as in a sinus infection, can also appear brownish.
One other possible culprit? Tobacco. If you chew tobacco or smoke cigarettes (especially hand-rolled), you may notice the tobacco staining your mucus a yellowish brown. Same goes for just about any other restricted substance that you can chew or smoke.
Snot Color #7: Gray Or Black Mucus
Morgan Swofford for LittleThings
Nobody wants to find black mucus on their hankie. Still, it’s usually not a big deal.
Black mucus is often the result of inhaling a foreign substance, like smoke, soot, or ash. This may happen if you’ve been smoking or have been around smokers (or if you’ve been in any other environment where you may have inhaled fine, dark particles).
Finding ashy snot just once or twice is nothing to worry about, but you should try to cut back on situations where you might inhale these particles. You could even consider wearing a breathing mask. Habitually inhaling foreign substances is not good for your body.
In some rare cases, black or gray mucus may also signal that there’s a fungus causing your sinus issues. Go see a doctor, just to be safe.
11-14-17
DEBUNKING MYTHS ABOUT THE FLU SHOT
No more excuses!

You start to see the signs in August and September – “Flu Shots Here”. They are at every pharmacy and medical facility, and your employer may even host a flu shot clinic at work. Some people are on board right away; others have a bevy of excuses why they won’t get a flu shot. “I got a shot last year and got sick from it the next day.” Or “I never get a flu shot and I never get sick.” Or “I’m allergic to eggs so I can’t get the shot.”
Let’s address each of these statements individually because it is important for as many people as possible to become vaccinated:
Can you get the flu from a flu shot?
The short answer is no. First, it takes two weeks for the flu virus to incubate and cause symptoms. If you have the flu shortly after you get a shot, you most likely contracted it somewhere else within the past two weeks and you were going to get sick anyway. Second, flu vaccines are made one of two ways:
Using an “inactivated” viruses which make it non-infectious
Using absolutely no flu viruses at all
Both of these methods result in a vaccine which cannot cause the flu.
If you get the flu more than two weeks after the shot, you most likely contracted a strain of the virus not covered by the shot you received. The CDC formulates the vaccine based on the most likely strains to hit the US in any given year. It is an educated guess, but sometimes another strain finds its way into the US.
If I have never had the flu before, why would I need a flu shot now?
Just because you have never had the flu (or think you have never had the flu), it is possible this year could be the year. Strains of the flu virus are mutating continually and what has not made you sick in the past, may make you sick now. Additionally, you move through the world and interact with other human beings who may not be as resistant to viruses as you think you are. When you contract the flu, you are contagious from around one day before you have symptoms until five to seven days after. Any hard surfaces you get your germs on during this time can remain contagious for up to 48 hours. To be blunt, even when you don’t feel sick, you may be sick and can make others around you sick.
Can I get a flu shot if I am allergic to eggs?
One of the standard questions on the wellness sheet most places have you sign before the shot asks if you are allergic to eggs. The reason is they are covering themselves because most flu vaccines are produced using an egg-based manufacturing process and contain a small amount of egg protein called ovalbumin; however, unless you have severe allergic reactions to eggs (other than simple hives) like respiratory or other reactions requiring medical intervention, you can receive any flu vaccine. Even if you have had a severe reaction to eggs you can still get a flu vaccine, but it is recommended you receive the vaccine in a medical facility equipped to handle a severe allergic reaction and be sure to notify the person administering the vaccine of your allergy. The only people who should not receive a flu vaccine are those who have had a severe reaction to flu vaccines in the past.
OK, maybe I didn’t get the flu from the flu shot, but I still don’t want to get one. Why should I?
As mentioned earlier, we all interact with one another and the number of people we “touch” is exponential. Door knobs, counters, office furniture, grocery carts, and other public shared surfaces, in addition to person-to-person contact, can spread the flu virus. Have you ever been on an airplane with someone who is coughing, sneezing, etc and inwardly groaned because you just knew whatever they had was making its way around the enclosed cabin?
When you get a flu shot, you are not just protecting yourself, you are helping protect everyone around you. Some people are legitimately not able to get the flu shot due to a compromised immune system or advanced age. The very young (babies under 6 months of age are not old enough for the vaccine and are extremely at risk) and the very old are of particular concern.
People who are cardiac compromised run a larger risk of suffering a cardiac event as the result of contracting the flu and should always get a flu shot. In fact, incidences of cardiac visits to hospitals increase during the peak of flu outbreaks.
If a family member contracted Guillain-Barre Syndrome after a flu shot, should I not get one?
Guillain-Barre syndrome (GBS) is exceptionally rare and occurs in only 1 or 2 people per million vaccinated. In fact, a person prone to getting GBS is more at risk for getting it after having the flu than after receiving the vaccine. There is no evidence to suggest it is hereditary (which is why it is called a “syndrome” and not a “disease”). GBS is a very serious condition and can have a long recovery time. It is understandable someone who has watched a loved one go through all the stages of GBS, many of which are quite painful, would want to avoid enduring the same circumstances. If a family member has had GBS and you are concerned about getting a flu shot, it is recommended you speak with your doctor about it and decide with them what the best course of action is for you.
I’m still not convinced, what can I do to avoid getting the flu besides a shot?
If you still decide not to receive a flu shot, please take precautions during flu season. Eat healthily and stay hydrated, wash your hands often (especially when you are out in public, and definitely before eating or touching your mouth or nose), disinfect surfaces often in your home and office. If you start feeling ill, minimize your contact with others. If you can stay home from work, you should stay home from work – your co-workers will thank you. Staying home and resting is your best bet for a quick recovery anyway.
Stay healthy!
Your child should not be at school if he/she has any of these symptoms:
– Has a 100 degree or over temperature or needs fever reducing medication
– Must have a normal temperature for 24 hours or more without medication
– Examples: Tylenol, Advil, Motrin, Ibuprofen, etc.
– Has been taking antibiotics for less than 24 hours
– Vomiting/diarrhea- Stay at home for 24 hours after vomiting or diarrhea
– Must be able to eat and drink before coming back
– Rash—if rash is over large part of body or is oozing or contagious
– Red eye—if white part of eye is red and there is yellow or green crusty or gooey stuff in eye or has conjunctivitis. They must stay at home for 24 hours or more after medication has started.
